Every cell in the human brain depends on a continuous flow of oxygen-rich blood. When that flow is interrupted, even for a short time, brain tissue begins to die. This process is known as hypoxic or anoxic brain injury—a silent emergency that can change the course of a person’s life in moments.
- Understanding Hypoxia and Anoxia
- What Happens When the Brain Lacks Oxygen
- Common Causes of Hypoxic and Anoxic Brain Injury
- 1. Cardiac Arrest
- 2. Respiratory Failure
- 3. Drowning or Near-Drowning
- 4. Strangulation or Suffocation
- 5. Stroke and Blood Vessel Blockage
- 6. Anesthesia or Surgical Complications
- 7. Carbon Monoxide Poisoning
- Areas of the Brain Most Affected
- Symptoms of Hypoxic or Anoxic Brain Injury
- Diagnosis: How Doctors Detect Oxygen Deprivation
- Treatment and Early Management
- Rehabilitation and Recovery
- Prognosis and Long-Term Outlook
- Prevention: Reducing the Risk of Oxygen Deprivation
- The Takeaway
Unlike traumatic brain injuries caused by impact, these injuries arise from internal medical crises such as cardiac arrest, drowning, respiratory failure, or stroke. Because oxygen loss affects the entire brain, the consequences are often severe and widespread.
Understanding Hypoxia and Anoxia
The difference between hypoxia and anoxia lies in how complete the oxygen loss is:
- Hypoxia means the brain is receiving too little oxygen to meet its needs.
- Anoxia means a total absence of oxygen to brain tissue.
Both can cause irreversible damage, but anoxia acts more quickly and destructively. Neurons—the brain’s most sensitive cells—begin to die within four to five minutes without oxygen. Prolonged deprivation can lead to widespread cell death, swelling, and coma.
What Happens When the Brain Lacks Oxygen
The brain’s metabolism is built around oxygen. It uses it to produce energy through cellular respiration. When oxygen is cut off, cells switch to anaerobic metabolism, producing lactic acid and triggering a toxic cascade that disrupts membranes and electrical activity.
This process sets off a chain reaction:
- Loss of consciousness occurs within seconds.
- Irreversible damage can begin after several minutes.
- Swelling and inflammation follow, worsening the injury.
- Secondary complications, such as seizures or elevated intracranial pressure, may develop even after oxygen is restored.
This combination of primary and secondary injury is why hypoxic and anoxic events require rapid emergency response and prolonged rehabilitation.
Common Causes of Hypoxic and Anoxic Brain Injury
These injuries occur in many different medical and environmental situations. Some of the most frequent include:
1. Cardiac Arrest
When the heart stops pumping, blood flow to the brain ceases instantly. Even if circulation is restored, the temporary lack of oxygen often leads to anoxic injury. This is one of the most common causes in adults.
2. Respiratory Failure
Conditions such as asthma attacks, choking, severe pneumonia, or opioid overdose can prevent enough oxygen from reaching the brain. Prolonged apnea (not breathing) leads rapidly to injury.
3. Drowning or Near-Drowning
Inhalation of water blocks oxygen exchange in the lungs. Even brief submersion—especially in children—can lead to lasting hypoxic brain damage.
4. Strangulation or Suffocation
These events cut off air supply to the lungs and circulation to the brain, leading to quick and severe anoxia.
5. Stroke and Blood Vessel Blockage
While most strokes are localized, large-vessel blockages or hemorrhages can deprive large areas of the brain of oxygen and blood flow.
6. Anesthesia or Surgical Complications
Errors during anesthesia, intubation, or cardiopulmonary bypass can reduce oxygen levels. Fortunately, these are rare with modern monitoring.
7. Carbon Monoxide Poisoning
Carbon monoxide binds to hemoglobin more strongly than oxygen, starving brain tissue even when breathing appears normal.
Areas of the Brain Most Affected
Some regions of the brain are more vulnerable than others to oxygen deprivation, particularly those with high metabolic demand:
- Hippocampus: Memory formation and learning
- Cerebral cortex: Thinking, awareness, and sensory processing
- Cerebellum: Coordination and balance
- Basal ganglia: Motor control and movement regulation
The pattern of damage often explains why survivors may struggle with short-term memory, attention, and physical coordination even after apparent recovery.
Symptoms of Hypoxic or Anoxic Brain Injury
Symptoms vary depending on the duration and severity of oxygen loss. They can range from mild confusion to complete unconsciousness.
Mild to Moderate Cases
- Headache, dizziness, or disorientation
- Difficulty concentrating or forming new memories
- Fatigue and slowed thinking
- Short-term speech or coordination problems
- Mood swings or anxiety
Severe Cases
- Prolonged unconsciousness or coma
- Seizures
- Loss of muscle control or paralysis
- Visual or auditory impairment
- Profound memory loss and personality changes
The severity of these symptoms often evolves over hours or days after the initial event, as swelling and chemical changes continue in the brain.
Diagnosis: How Doctors Detect Oxygen Deprivation
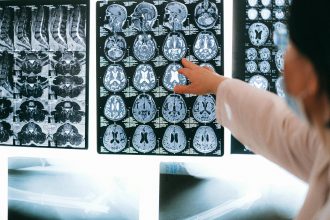
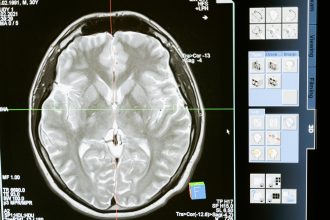
Diagnosis begins with identifying the underlying cause of the oxygen loss. Physicians use several methods to assess the extent of injury:
- Neurological examination: Evaluates responsiveness, reflexes, and motor function.
- CT or MRI scans: Reveal swelling, lesions, or diffuse injury patterns.
- EEG (electroencephalogram): Measures brain wave activity and helps determine consciousness level.
- Blood oxygen and metabolic tests: Indicate how well the brain and other organs are being perfused.
In many cases, imaging studies are repeated over time to track progress or deterioration.
Treatment and Early Management
There is no way to “undo” oxygen deprivation, so the focus of medical care is to stabilize the patient and minimize secondary injury.
Emergency Treatment
- Restoring oxygen and circulation as quickly as possible
- Maintaining body temperature and blood pressure
- Preventing seizures and brain swelling
- Using mechanical ventilation if necessary
Hospital and ICU Care
- Continuous brain activity monitoring
- Administration of medications to reduce swelling or manage seizures
- Oxygen therapy and controlled ventilation
- Support for heart, lungs, and kidneys during recovery
Some cases may involve therapeutic hypothermia, a controlled cooling technique that slows metabolism and protects brain tissue from further injury after cardiac arrest.
Rehabilitation and Recovery
Rehabilitation begins once the patient is stable. Recovery can be slow and unpredictable, often requiring months or years of therapy.
Common Rehabilitation Approaches
- Physical therapy: To rebuild strength, posture, and coordination
- Occupational therapy: For daily living activities and independence
- Speech and language therapy: For communication and swallowing issues
- Cognitive rehabilitation: To improve attention, memory, and reasoning
- Neuropsychological counseling: To manage emotional and behavioral changes
Family and caregiver support are essential. Even small improvements—such as following commands, speaking, or recognizing loved ones—mark important steps in recovery.
Prognosis and Long-Term Outlook
Outcomes depend on how long the brain was deprived of oxygen and how quickly medical care was provided.
- Short-term hypoxia (under 3 minutes): Often reversible with mild deficits.
- Prolonged hypoxia (over 5 minutes): Typically leads to moderate or severe cognitive and physical impairment.
- Extended anoxia: May result in coma, persistent vegetative state, or death.
Some survivors regain remarkable function through neuroplasticity—the brain’s ability to rewire itself—but others face lifelong challenges requiring 24-hour care.
Prevention: Reducing the Risk of Oxygen Deprivation
While some causes are unpredictable, many cases can be prevented through awareness and timely intervention:
- Learn CPR and basic life support. Immediate response during cardiac arrest or drowning dramatically improves outcomes.
- Install carbon monoxide detectors in homes and workplaces.
- Treat respiratory conditions promptly and manage chronic illnesses such as asthma or heart disease.
- Practice water safety with supervision and flotation devices.
- Avoid opioid misuse and seek treatment for substance dependency.
These simple steps can mean the difference between full recovery and lasting brain injury.
The Takeaway
Hypoxic and anoxic brain injuries remind us how dependent the brain is on oxygen—and how quickly things can change when that supply stops. But they also highlight the power of rapid intervention, skilled rehabilitation, and the human capacity for recovery.
Every second counts when oxygen is lost, and every effort toward prevention, education, and care helps protect the most vital organ we have.