When someone shows signs of a brain injury, quick and accurate diagnosis is essential. Doctors must determine how severe the injury is, what areas of the brain are affected, and what treatments are needed. Diagnosis combines medical history, physical and neurological exams, and imaging tests. In some cases, specialized assessments are also required.
The process helps doctors decide whether immediate surgery is needed, whether hospitalization is required, and what rehabilitation plan will give the best chance for recovery.
Initial Assessment
Diagnosis often begins at the scene of the injury or in the emergency department. First responders and doctors focus on:
- Stabilizing vital signs — ensuring breathing and blood flow are intact.
- Level of consciousness — using the Glasgow Coma Scale (GCS), which measures eye, verbal, and motor responses.
- Mild injury: GCS score of 13–15
- Moderate injury: GCS score of 9–12
- Severe injury: GCS score of 3–8
This quick evaluation guides the urgency of treatment.
Neurological Examination
Once stabilized, a more detailed neurological exam checks:
- Reflexes and motor function
- Coordination and balance
- Speech and language ability
- Pupil response to light
- Cognitive status — orientation, memory, and problem-solving
These tests help identify which areas of the brain may be involved.
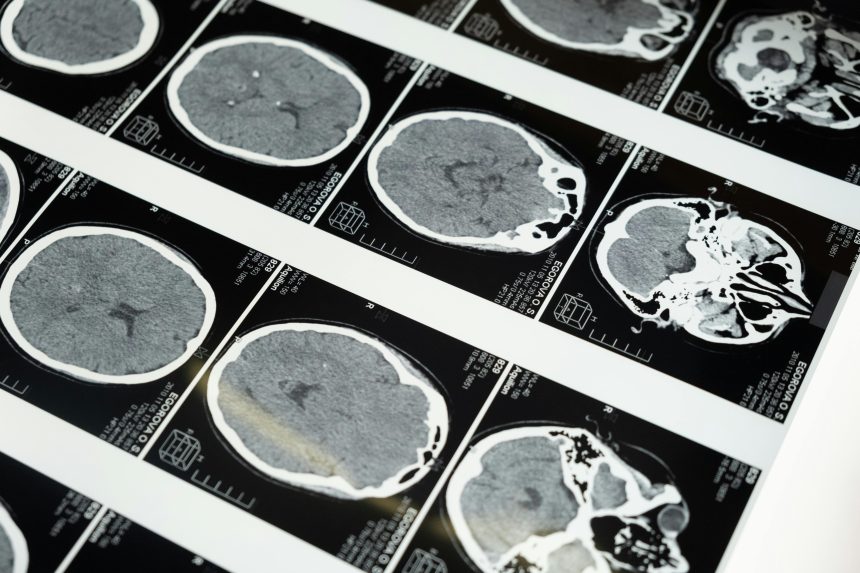
Imaging Tests
Imaging is one of the most important diagnostic tools in brain injury care.
- CT Scan (Computed Tomography): The first-line scan in emergencies. CTs quickly reveal fractures, bleeding, swelling, and blood clots.
- MRI (Magnetic Resonance Imaging): Provides more detailed images of brain tissue, useful for detecting subtle damage, diffuse axonal injury, or long-term changes.
- Advanced Imaging (fMRI, DTI, PET): Used in research and specialized clinics to study brain function and connectivity.
Neuropsychological Testing
Not all brain injuries are visible on scans. Cognitive and emotional symptoms may require specialized testing. Neuropsychologists use standardized tools to evaluate:
- Memory
- Attention and concentration
- Processing speed
- Problem-solving and reasoning
- Emotional and behavioral regulation
These results guide rehabilitation plans and school/work accommodations.
Other Diagnostic Tools
In certain cases, additional tests are used:
- EEG (Electroencephalogram): Detects abnormal brain activity and seizures.
- Intracranial Pressure (ICP) Monitoring: Measures swelling inside the skull in severe TBIs.
- Blood Tests (emerging research): Scientists are developing biomarkers to detect brain injury chemicals in the blood.
Challenges in Diagnosis
Not all brain injuries are immediately obvious. Mild TBIs may show normal CT or MRI results but still cause significant symptoms. This makes clinical judgment and patient history critical parts of diagnosis.
Similarly, acquired brain injuries such as stroke may require rapid differentiation between clot-related and bleed-related events, since treatment differs.
Why Early Diagnosis Matters
Accurate diagnosis is the foundation of effective treatment. Early detection allows doctors to:
- Prevent secondary damage (bleeding, swelling, oxygen loss)
- Begin timely rehabilitation
- Provide families with realistic expectations
- Monitor for complications like seizures or hydrocephalus
Conclusion
Diagnosing a brain injury is a multi-step process involving exams, imaging, and sometimes specialized testing. Whether mild or severe, early recognition and accurate diagnosis improve recovery outcomes and help families plan for rehabilitation and long-term care.
For more details on treatment after diagnosis, see Brain Injury Rehabilitation.