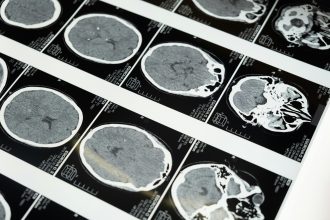
Diagnosing brain injury has long depended on imaging and clinical observation — CT scans for bleeding, MRIs for structural damage, and bedside exams for cognitive function. Yet even the best scans can miss microscopic or biochemical changes that alter how the brain works. That’s where biomarkers and new diagnostic technologies are transforming the field.
Researchers are developing tests that detect brain injury at the molecular level, sometimes within minutes of trauma. These tools promise earlier, more precise diagnoses and could one day guide treatment the way blood tests already do for heart attacks or infections.
What Are Biomarkers?
A biomarker is a measurable substance in the body that signals injury or disease. In brain injury, biomarkers are typically proteins released from damaged neurons, glial cells, or supporting tissue. When brain cells are injured, fragments of these proteins enter the bloodstream or cerebrospinal fluid — and their presence can indicate both severity and type of injury.
Key biomarkers currently under study include:
- GFAP (Glial Fibrillary Acidic Protein) – released when astrocytes, a type of brain support cell, are damaged.
- UCH-L1 (Ubiquitin C-Terminal Hydrolase L1) – reflects neuronal injury.
- S100B – associated with blood–brain barrier disruption and glial damage.
- Tau and Neurofilament Light (NfL) – linked to axonal injury and neurodegeneration.
Blood tests measuring GFAP and UCH-L1 have already gained FDA clearance for evaluating mild traumatic brain injury (mTBI), offering a safer, faster alternative to routine CT scans in selected patients.
Imaging Beyond the Visible
Traditional imaging shows structure — not always function. Advanced imaging methods now reveal subtle brain changes that standard scans may overlook:
- Diffusion Tensor Imaging (DTI) traces water movement along white-matter tracts, detecting micro-damage to axons.
- Functional MRI (fMRI) maps brain activity during tasks, helping researchers understand post-injury cognition and emotion.
- Magnetoencephalography (MEG) and Quantitative EEG (qEEG) measure electrical and magnetic activity, showing how the brain communicates after trauma.
These techniques help bridge the gap between visible injury and invisible symptoms — such as memory loss, fatigue, or mood change — that patients often experience long after the scans look “normal.”
Artificial Intelligence and Digital Diagnostics
AI is rapidly becoming part of the diagnostic toolkit. Machine learning systems can analyze thousands of imaging patterns or physiological signals to predict injury severity, recovery potential, and even the risk of complications such as post-traumatic epilepsy.
At the same time, wearable sensors and mobile apps are entering clinical trials. They track eye movements, speech, reaction time, and balance — metrics that can indicate concussion or delayed recovery. Combined with biomarker data, these tools could create a comprehensive, real-time picture of brain health.
The Promise and the Caution
While biomarker testing and AI-driven diagnostics offer tremendous potential, they remain complementary to — not replacements for — clinical judgment. Factors such as age, preexisting conditions, and timing of the test still affect results. More research is needed to set universal thresholds, improve reliability, and make these tools affordable for routine care.
But progress is steady. In the near future, emergency departments may use a single drop of blood to decide who needs imaging, who can safely rest, and how to monitor recovery with precision never before possible.
The Takeaway
The next generation of brain injury diagnostics is emerging from the lab into clinical reality. From protein markers and advanced imaging to AI analysis, these tools are reshaping how doctors understand, diagnose, and manage brain injury — moving from visible damage to molecular insight. For patients and families, that means faster answers, safer care, and a clearer path toward recovery.